Next time you feel the sun warming up your skin, know that vitamin D production is underway! Vitamin D is more than just a vitamin, it’s an essential key to healthy behavior, cognition, and well-being. Without it, things can go haywire! In fact, people that are vitamin D deficient exhibit anxiety and depressive-like behaviors[1]. Due to its impact on behavior and cognition, vitamin D deficiency is increasingly becoming a public health issue[2][3]. So, it’s truly a vitamin that shouldn’t be neglected!
Classically, vitamin D has been associated with bone health and calcium-phosphorus homeostasis, being a key player in the skeletal system, kidneys, and intestines. Nowadays, medicine has shown that many diseases are becoming epidemiologically associated with vitamin D deficiency, including infectious diseases, obesity, neuromuscular disorders, autoimmune diseases, cancer, and neuropsychiatric disorders[1]. In fact, vitamin D deficiency has been associated with a vast array of behavioral and neurochemical brain alterations.
This article will expand upon how vitamin D supplementation and deficiency in animal disease models are implicated in serious conditions, including autism, diabetes, and Alzheimer’s disease. Special note and attention will be taken of the behaviors and cognitive abilities observed during the experiments highlighted. Let’s begin by taking a closer look at the interplay between mood, vitamin D, and anxiety.
Vitamin D, Anxiety, Mood, and Depression
Did you know that there is a deep, complicated connection between the sun-vitamin and mood?
In a recent study in overweight and obese subjects, vitamin D supplementation alleviated the participant’s symptoms of depression[4].
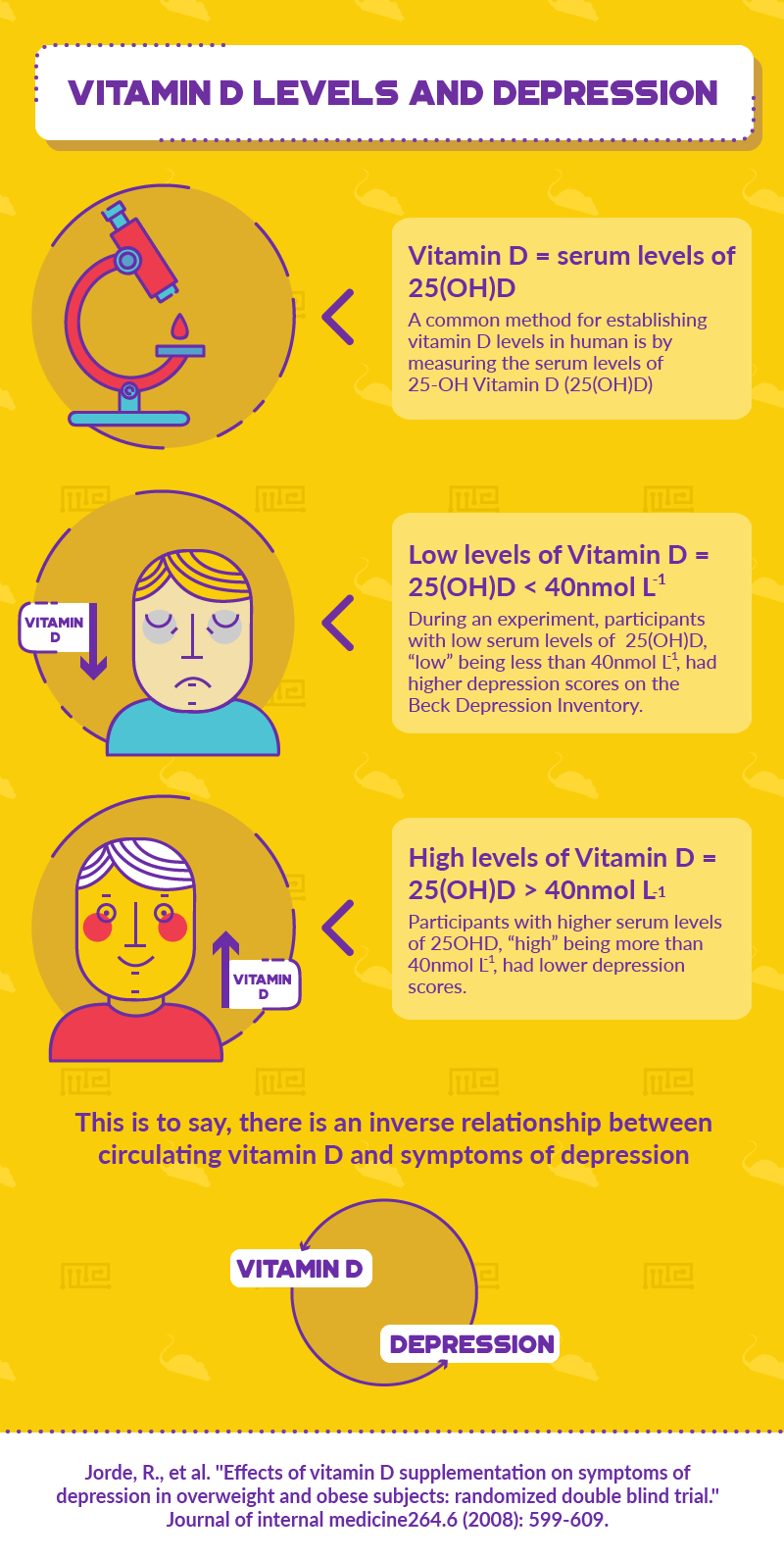
The researchers took note of the vitamin D levels by measuring the participants’ serum levels of 25-hydroxyvitamin D (25(OH)D), a common method for establishing vitamin D levels available in humans. The participant with l ls of 25(OH)D, “low” being less than 40nmol L-1, had higher depression scores on the Beck Depression Inventory. On the other hand, participants with higher serum levels of 25(OH)D, “high” being more than 40nmol L-1, had lower depression scores. Therefore, there is an inverse relationship between circulating vitamin D and symptoms of depression[4].
This antidepressant effect has also been extended to a clinical population with fibromyalgia. When studying a group of patients with clinical fibromyalgia, it was established that 56% of the patients were vitamin D insufficient and about 13% were deficient. Of the entire sample, the vitamin D insufficient fibromyalgia patients exhibited the most depression- and anxiety-related symptoms[5]. The fact that more than half of the sample had insufficient levels of vitamin D and subsequently displayed the highest depressive- and anxiety-related symptoms means that vitamin D is definitely involved somehow in anxiety, mood, and depression.
In animals, vitamin D deficiency has been associated with anxiety and depressive-like behavior, as well as impaired learning and memory[6]. To get a closer look at the relationship between anxiety-related behavior and vitamin D, a group of researchers made use of the Elevated Plus Maze Test. In their experiment, the vitamin D deficient mice had a reduced number of crossings in the open arms of the maze, but not in the closed arms, meaning that they were producing anxiety-like behavior by avoiding open spaces. Furthermore, in the Open Field Test, the vitamin D deficient mice were hyperactive, crossing more squares and traveling more distance than the controls. Such hyperactivity is associated with anxious behavior and restlessness[6].
In a different experiment, focusing on the effect of induced vitamin D deficiency in mothers and their future offspring, similar hyperlocomotion patterns were observed. Increased exploratory levels were noted in the vitamin D deficient offspring during the Hole Board Test wherein frequency of head dipping is measured as the exploratory behavior of interest. The researchers concluded that vitamin D deficiency contributes to behavioral changes and affects development in such a way that may lead to neuropsychiatric outcomes.
Still, further research needs to be done in order to establish how vitamin D administration (and also deficiency) affect and are implicated in mood disorders, as well as anxiety. For example, it remains to be established how vitamin D affects depressed patients’ hypothalamic-pituitary-adrenal axis’ response to stressful events and whether it would have any impact on monoamine function[7].
Vitamin D Increases Sociability in Autism Prone Offspring
Although a complete understanding of autism spectrum disorder (ASD) still remains elusive, two possible causes or influential factors for the disorder’s pathophysiology have been put forth. Viral infection during pregnancy and vitamin D deficiency have each been established as capable of increasing the likelihood of an ASD diagnosis. Animal models have revealed that this may be due to maternal immune activation (MIA) which involves oxidative stress and multiple cytokine-related inflammatory events.
Vitamin D deficiency has already been linked with autism-related dysfunctions during language and cognitive development in children[8]. Similar behavioral profiles have been noted in offspring that had a prenatal viral infection. Both vitamin D deficiency and viral infections lead to inflammation and scientists are currently exploring the possibility of the convergence of these inflammatory pathways as responsible for causing psychiatric and brain abnormalities.
A group of researchers wanted to see the effects that vitamin D would have on autism-related phenotypes. So they used the MIA mouse model and created several experimental conditions in order to test their theory that vitamin D administration would be able to prevent some of the behavioral dysfunctions associated with ASD.
To induce MIA, the researchers used the most commonly used MIA animal model: gestational exposure to a certain viral synthetic analog, polyriboinosinic-polyribocytidylic acid (Poly(I:C)). This viral mimic is a double-stranded RNA which induces, in both the mother and the fetus, a cytokine-related viral-like acute-phase. This model was initially developed and introduced as a schizophrenia model but has since been reproduced for uses relating to ASD[9].
The researchers used several experimental groups to test out their hypothesis that vitamin D supplementation would ameliorate the behavioral and cognitive problems brought about by viral Poly(I:C)-induced ASD.
To create the experimental conditions, researchers subcutaneously injected pregnant dams with either a vehicle solution (to serve as the control group) or with 1α,25 dihydroxy vitamin D3, a hormonally active form of vitamin D (VitD). Then, the same rats were intravenously injected with either a saline solution or poly(I:C). So, there were four groups in total:
- Poly(I:C) + VitD
- Poly(I:C) + Vehicle (VEH)
- Saline solution (CON) + VEH
- CON + VitD
For this particular experiment and model, the Elevated Plus Maze test showed that there were no group differences when it came to behaviors that connote anxiety. All the groups showed similar performance in the open arm distance traveled, in the percent of time spent in the open arms, and the total distance traveled. So, all the groups had about the same levels of anxiety throughout the experiment.
What was remarkable, however, was the behavior exhibited during the Y-Maze by the poly(I:C) mice which would be destined for ASD-like behaviors due to their prenatal exposure to the vital synthetic analog. The baby mice that were exposed to the poly(I:C) and given the VitD supplement showed a reduction in ASD symptoms when it came to social interactions as demonstrated by the subsequent increase in relative time spent with a new, unfamiliar mouse. Unsurprisingly, the young poly(I:C) mice which were given a vehicle solution instead retained the ASD-like behaviors and showed social avoidance. The stark differences between the two poly(I:C) groups (one given a VitD supplement and the other not) suggests that VitD supplements have the ability to block the negative effects associated with MIA-related ASD on social cognition and behavior[10].
The introduction of vitamin D to the MIA autism-phenotype disease model demonstrated noteworthy results which should be further explored by other researchers interested in psychiatric diseases, mental health, behavior, and well-being.
Vitamin D Intake Improves Memory in Diabetic Mice
Diabetic mice have also been documented to show behavioral responses to vitamin D. To study the interplay between vitamin D and learning and memory impairment in diabetic mice, a group of scientists made use of the streptozotocin-induced diabetes animal model.
To measure the animals’ learning and memory abilities, the researchers used an Active/Passive Avoidance Shuttle Box which is the apparatus needed to run a passive avoidance test. In the passive avoidance test, the animals are expected either to avoid performing a particular behavior (the “passive” component) or to perform a particular behavior (the “active” component), in order to stay clear of the aversive, experimental stimuli.
The trials began with placing the mouse in the light area of the shuttle box and each time the mouse went into the dark area, it would receive a foot shock! So, the mice had to learn to override their innate preference for the dark (mice and rats prefer dark areas over light ones).
In general, the diabetic mice supplemented with vitamin D exhibited different learning patterns and behaviors from the control diabetic mice which were not given treatment. The vitamin D supplemented diabetic mice had a shorter initial latency than the non-treated diabetic group, meaning that they had better learning abilities. In fact, the supplemented mice performed at the level of the healthy non-diabetic control group. Furthermore, when the diabetic mice were given vitamin D, they ended up spending the least amount of time in the dark compartment out of all of the groups! The fact that the vitamin-D treated diabetic group had the least number of entries in the dark room shows that they were most able to retain the trained behaviors they had learned[11].
In humans, diabetes is associated with memory deficits, but also an array of other conditions, such as depression. In a randomized double-blind study, overweight and obese people that were given a high dose of vitamin D supplements had ameliorated or decreased symptoms of depression after year-long supplementation as revealed by changing scores in the Beck’s Depression Inventory[12].
Therefore, vitamin D is able to affect many domains of behavior and cognition, including learning, memory, and mood.
Neuroprotective Effects of Vitamin D3 in Alzheimer’s
A specific form of vitamin D has been demonstrated to have neuroprotective properties in an experiment making use of an Alzheimer’s animal model induced by bilateral icv colchicine injection.
The mice were divided into four groups for experimental purposes:
- Rats in the healthy control group were injected with artificial cerebrospinal fluid
- Alzheimer’s disease-induced rats as induced by bilateral icv colchicine injection, receiving no treatment
- Rats treated with vitamin D3 before Alzheimer’s induction and then again after the Alzheimer’s induction (i.e. receiving both pre- and post-treatment of vitamin D)
- Alzheimer-induced rats with only post-induction treatment of vitamin D3
Such an experimental design takes into account whether vitamin D3 intake before the onset of the disease would have any effect on the outcome and course of the pathophysiology.
The researchers found, using the Morris Water Maze, that the controls and both groups treated with vitamin D3 were able to learn quickly to swim to the Morris Water Maze platform, a behavior which the untreated Alzheimer’s-induced mice were unable to do. The untreated Alzheimer’s-induced mice showed a significant difference than the controls, demonstrating that the animal induced model was working in establishing the memory deficits.
Furthermore, following the training period, retention latencies (the ability to remember after a long period of time has passed) were measured. The untreated Alzheimer’s-induced mice had significantly higher latency times than both of the vitamin D3 treated groups and the control, meaning that they were unable to preserve intact spatial memories as well as the other groups could.
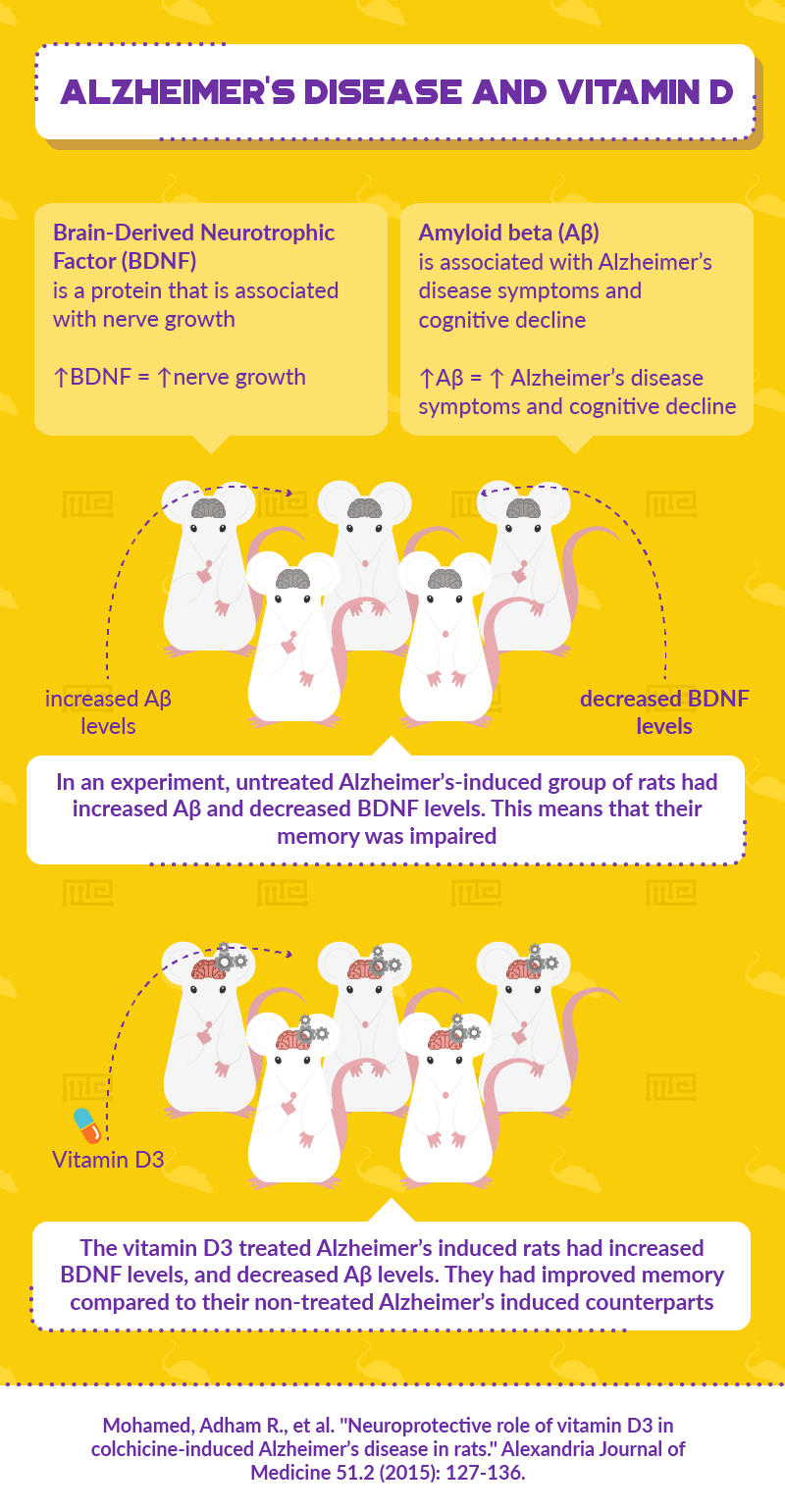
To supplement the behavioral findings, the researchers ran biochemical measurements of brain-derived neurotrophic factor (BDNF) and amyloid beta (Aβ) peptide of the rats’ brain tissues. While BDNF is a protein that is associated with nerve growth, Aβ is associated with Alzheimer’s disease symptoms and cognitive decline. The brain tissue analysis revealed that the untreated Alzheimer’s-induced group of rats had increased Aβ and decreased BDNF levels when compared to the control group. The vitamin D3 treated Alzheimer’s induced rats, on the other hand, had increased BDNF levels, and decreased Aβ levels compared to their non-treated Alzheimer’s induced counterparts.
This experiment, combining facets of anatomical biology and behavioral science, shows the impact of vitamin D3 treatment on the brain’s physiology and that the behavioral and cognitive symptoms associated with Alzheimer’s disease may be somehow related with vitamin D intake.
Conclusion
Vitamin D has proven to be quite important for health and able to affect behavior. For example, in animal studies, vitamin D3 supplementation has been shown to be able to increase BDNF and reverse aβ levels, subsequently affecting memory. Such findings are quite tremendous and remarkable, given the implications for conditions such as dementia or Alzheimer’s disease.
Among many other interesting findings, vitamin D administration has also been demonstrated to reverse some of the learning deficits associated with diabetes in diabetes-induced animal models. In the human population, a link between vitamin D supplementation, anxiety, and depression has already been established in those with fibromyalgia or obesity.
Despite the potent effects listed to date, much about vitamin D remains to be established. More research should be done to study this vitamin’s effect in a variety of other disease models. Also, further investigation is warranted, in order to uncover the exact nature of the interaction between vitamin D, anxiety, and depression.
References
- Di Somma, Carolina, et al. “Vitamin D and Neurological Diseases: An Endocrine View.” International journal of molecular sciences 18.11 (2017): 2482.
- Wilson, Louise R., et al. “Vitamin D deficiency as a public health issue: using vitamin D 2 or vitamin D 3 in future fortification strategies.” Proceedings of the Nutrition Society76.3 (2017): 392-399.
- Adams, John S., and Martin Hewison. “Update in vitamin D.” The Journal of Clinical Endocrinology & Metabolism 95.2 (2010): 471-478.
- Jorde, R., et al. “Effects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: randomized double blind trial.” Journal of internal medicine264.6 (2008): 599-609.
- Armstrong, D. J., et al. “Vitamin D deficiency is associated with anxiety and depression in fibromyalgia.” Clinical rheumatology26.4 (2007): 551-554.
- Fu, Lin, et al. “Vitamin D deficiency impairs neurobehavioral development in male mice.” Physiology & behavior 179 (2017): 333-339.
- Bertone-Johnson, Elizabeth R. “Vitamin D and the occurrence of depression: causal association or circumstantial evidence?.” Nutrition reviews 67.8 (2009): 481-492.
- Fernell, Elisabeth, et al. “Autism spectrum disorder and low vitamin D at birth: a sibling control study.” Molecular autism 6.1 (2015): 3.
- Meyer, Urs, et al. “Towards an immuno-precipitated neurodevelopmental animal model of schizophrenia.” Neuroscience & Biobehavioral Reviews 29.6 (2005): 913-947.
- Vuillermot, Stephanie, et al. “Vitamin D treatment during pregnancy prevents autism-related phenotypes in a mouse model of maternal immune activation.” Molecular autism 8.1 (2017): 9.
- Hakiminia, Saeid. “Vitamin D improves learning and memory impairment in streptozotocin-induced diabetic mice.” Archives of Iranian medicine 18.6 (2015): 362.
- Jorde, R., et al. “Effects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: randomized double blind trial.” Journal of internal medicine264.6 (2008): 599-609.
- Mohamed, Adham R., et al. “Neuroprotective role of vitamin D3 in colchicine-induced Alzheimer’s disease in rats.” Alexandria Journal of Medicine 51.2 (2015): 127-136.
